
Q: Is Health Equity training mandatory for healthcare professionals licensed under Title 18 RCW in Washington State?
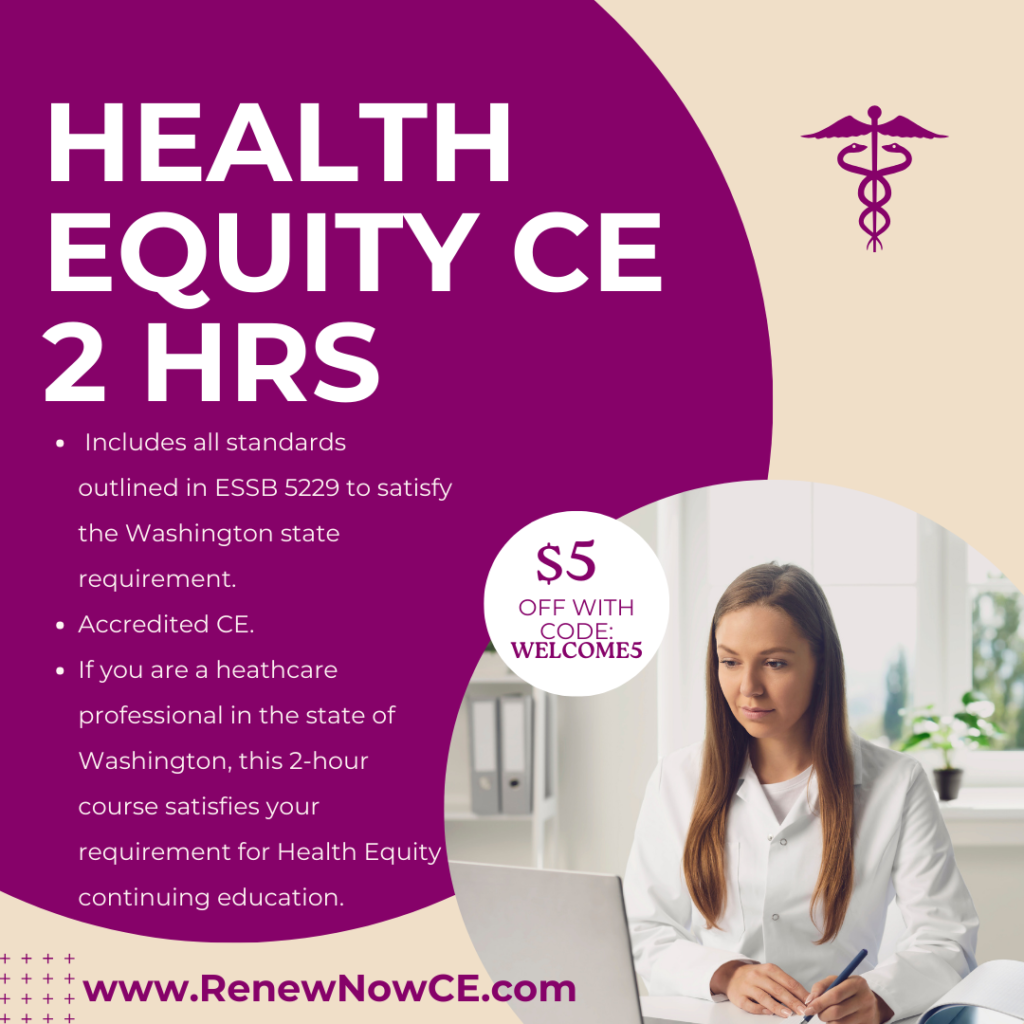
A: Yes. In Washington State, all healthcare professionals credentialed under Title 18 RCW (including RNs, LPNs, physicians, physician assistants, pharmacists, and mental health professionals) are required to complete 2 hours of Health Equity continuing education every four years. This mandate took effect by January 1, 2024 and is established under ESSB 5229, with rulemaking adopted by the Washington Department of Health pursuant to Title 18 RCW.
Renew Now CE provides an Instant Certificate for immediate license submission.
Health Equity CE Required in Washington State: A Comprehensive Guide for Healthcare Professionals
In response to ESSB 5229, the Washington Department of Health has mandated that healthcare professionals credentialed under Title 18 RCW must complete Health Equity CE required in Washington State. This new requirement aims to ensure that healthcare providers are equipped to address health disparities in their practice. By January 1, 2024, all licensees must complete 2 hours of health equity CE every four years.
The rule-making authority for each profession licensed under Title 18 RCW must adopt specific rules by 1/1/2024. This ensures that all healthcare professionals meet the new Health Equity CE required in Washington State standards.
Health Equity CE Requirements for Washington State Healthcare Professionals
As of December 22, 2023, all Title 18 RCW healthcare professionals must complete 2 hours of health equity CE. This requirement applies to registered nurses (RNs), licensed practical nurses (LPNs), physicians, physician assistants, pharmacists, mental health professionals, and other licensed healthcare providers.
Licensees must complete health equity CE at least once every four years, with specific renewal deadlines depending on their profession. The goal is to equip healthcare professionals with skills to address health disparities and provide equitable care.
Complete Your Washington Health Equity CE Now
The Washington Health Equity 2-Hour Course is available for $35 and provides CE credits for ADA CERP, ACCME, ANCC, CDR, ASWB, ACPE, AAPA, and APA. Meet the Health Equity CE required in Washington State by completing this course before your license renewal.
Health Equity CE Topics Covered in Washington State
The Washington State Health Department, in collaboration with various boards and commissions, has established minimum standards for health equity CE programs. The standards must address structural factors like bias, racism, and poverty, which contribute to health inequities. Topics in the course include:
- Recognizing Healthcare Disparities: Learn strategies for identifying and eliminating healthcare disparities at individual, institutional, and structural levels.
- Intercultural Communication Skills: Gain skills for effective communication with patients from diverse backgrounds, including working with interpreters and understanding cross-cultural communication styles.
- Implicit Bias Training: Learn strategies to reduce bias during patient assessment and diagnosis.
- Supporting Diverse Youth: Address the emotional well-being of children and youth from different cultural and socioeconomic backgrounds.
- Equity in Emerging Therapies: Ensure equity in care delivery, particularly regarding medical advancements and emerging therapies.
- Structural Competency: Develop skills to understand and address structural factors that affect health outcomes, including recognizing biases and developing structural humility.
- Cultural Safety: Gain an understanding of how a healthcare professional’s own culture impacts clinical interactions and service delivery, and learn how to engage in ongoing self-reflection and self-awareness.
The course assesses healthcare professionals’ ability to integrate health equity concepts into practice. This ensures the content is relevant and applicable to diverse patient populations.
Fulfill Your Health Equity CE Requirement in Washington State Today
Ensure compliance with the Health Equity CE required in Washington State by completing our 2-hour health equity course today. For just $35, you’ll receive CE credits for multiple accrediting bodies and meet the essential requirements for your license renewal. Don’t wait—take the next step toward enhancing your skills and advancing health equity in your practice.
Why Renew Now CE is the Smart Choice for Your License Renewal Continuing Education:
- Complete Your CE Requirements Today — No Subscriptions, No Stress
- Fully Accredited & Board-Accepted: ANCC-accredited and jointly accredited to provide CE for Nursing (ANCC), Medicine (ACCME), Pharmacy (ACPE), Dentistry (ADA CERP), and more.
- State-Mandated CE Compliance Guaranteed: Every course and package is built to meet your exact renewal-year requirements.
- Trusted by 100,000+ Clinicians Nationwide: Fast, accurate, and easy — with thousands of verified 5-star reviews.
- Buy Only What You Need: Choose a single course or a complete state bundle — no subscriptions, no upsells, no wasted hours.
- Instant Certificate: Finish your CE today and download your certificate immediately.
- Real Human Support: Get quick, reliable help from our U.S.-based team whenever you need it.
Additional Resources
- Washington Department of Health: Health Equity CE Information
Access official guidelines and updates on health equity continuing education requirements in Washington State. - ESSB 5229 Legislation: Read the Full Bill
Review the full text of ESSB 5229 to better understand the health equity education standards for healthcare professionals.
